Over long periods of time, elevated levels of cortisol can push us further down the road toward obesity, heart disease, depression, high blood pressure and unhealthy lifestyle behaviors. It is also true that individuals who are already coping with health issues are even more vulnerable to the negative effects of unmanaged long-term stress.
Cardiovascular system
Cardiovascular disease (CVD) is a major health concern for Americans, especially those over 60. CVD in older adults can impose a substantial burden in terms of disability, functional decline, mortality and health care costs, taking both a physical and emotional toll on those who are affected and their loved ones.
Below are some facts about seniors and heart disease in the United States:
- An estimated 121.5 million American adults (48%) have 1 or more types of cardiovascular disease (CVD). Of these, 43.7 million are estimated to be ≥60 years of age.
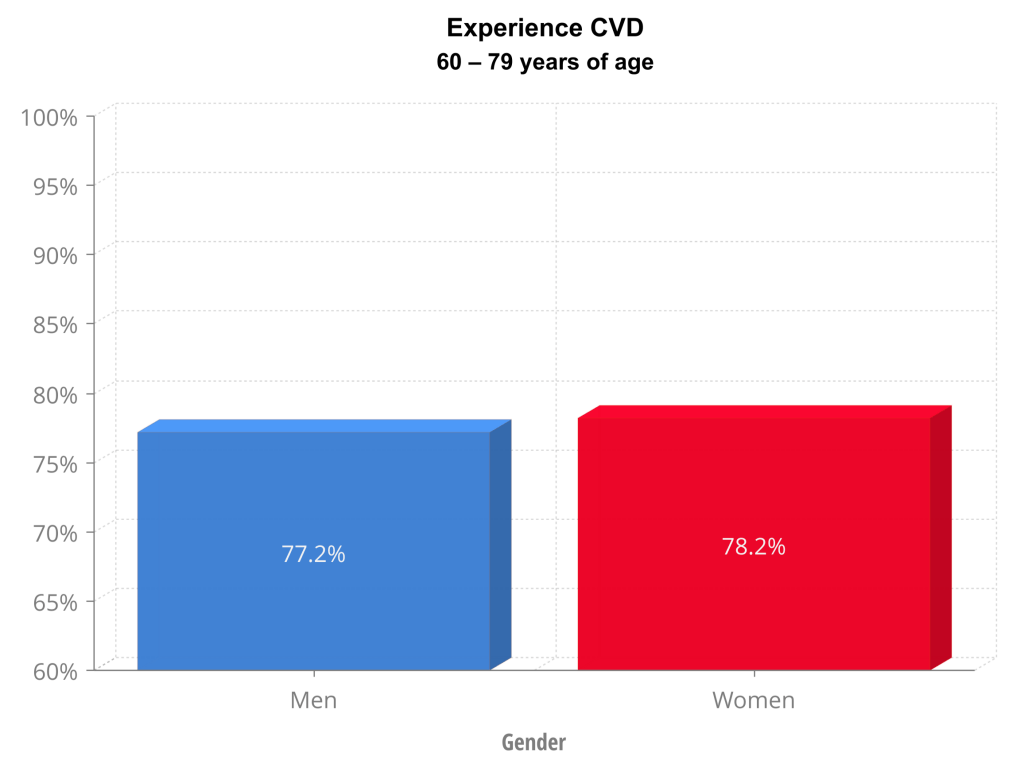
- For those between 60-79 years of age, 77.2% of men and 78.2% of women have some form of CVD.
- Of the 80+ age group, 89.3% of males and 91.9% of females experience CVD.
- The leading cause of mortality in adults ≥65 years of age is heart disease.
- Total direct and indirect annual costs for CVD and stroke in 2014-2015 were $150.2 billion for patients 65+.
Unmanaged, long-term stress can be a contributing factor in heart disease. The stress hormones that travel through the bloodstream can affect the blood vessels and heart. Adrenaline, also called epinephrine, causes the heart to beat faster, raising blood pressure. Over time, this can cause wear-and-tear on the cardiovascular system, potentially resulting in hypertension. Elevated cortisol can cause the inner lining of the blood vessels, the endothelium, to function abnormally. This dysfunction can be an early marker for atherosclerosis, the narrowing of the arteries caused by plaque build-up. All these changes in the cardiovascular system can increase the chance of heart attack or stroke.
According to a 2008 scientific review of clinical literature on heart disease and its link to psychological stress, “Although stressors trigger events, it is less clear that stress ‘causes’ the events” (Dimsdale, 2008). Managing unhealthy behaviors and attitudes can help counter the negative effects of stress on the cardiovascular system. o
Stress management can be key to unlocking better heart health for those who encounter chronic stress on a continual basis.
The digestive system
Have you ever experienced butterflies in your stomach in response to a stressful situation? Perhaps your digestive distress has been more serious, like heartburn, indigestion or even stress-related Irritable Bowel Syndrome (IBS). It is true that some of us feel the effects of stress in the gut and digestive system.
We understand when the brain recognizes a stressful event or situation, it activates the autonomic nervous system. The brain-gut connection is then triggered, which can cause a disturbance in the natural rhythmic contractions that move food through your digestive system, causing digestive distress in the form of heartburn and nausea, even leading to or worsening the symptoms of Irritable Bowel Syndrome or Inflammatory Bowel Disease. Research has even shown that stress can alter the composition and function of gut bacteria, which could affect the ease of digestion and overall health (Bridgewater, et al., 2017) (Lobionda, Sittipo, Kwon, & Lee, 2019).
Surprisingly, chronic stress can also affect the size of your waistline. Although some people find that they have a decreased appetite when experiencing stress, cortisol has been shown to increase appetite and cravings in some individuals. High levels of this hormone can cause visceral fat, the deep belly fat, to form. Visceral fat can increase the risk of chronic diseases like insulin resistance and heart disease.
Immune system
Stress hormones can impact immune cells in a variety of ways. Initially, the release of hormones like cortisol and adrenaline can help us prepare to fight off infection and to heal after injury, but stress that lasts for an extended period of time can dampen the function of some immune cells, and accelerate immune cell aging, making us more susceptible to infection and slowing the rate of healing (Damjanovic, et al., 2007). This lowering of white blood cells that accompanies long-term stress can put us more at risk for viruses, including the common cold and cold sores.
High stress levels can contribute to anxiety and depression, which may lead to higher levels of inflammation in the body. In the long term, sustained, high levels of inflammation lead to an overworked immune system that cannot properly protect us from illness.
Emerging research on the immune system’s response to chronic stress points to how stress management and strong interpersonal relationships can benefit day-to-day health, helping our bodies combat illness and speeding our healing after injury. The research is in sync with anecdotal evidence of how we often get sick during stressful times in our lives. Understanding how stress affects our biology can help us in our quest to manage stress on the most individualized and personal levels, giving us an opportunity to build our immune system.
Dental health
Stress can affect your oral health in many ways. Bruxism, or teeth grinding, which can happen during the day or at night, can be a result of chronic stress. Grinding and clenching teeth can be a major contributor to temporomandibular joint disease (TMJ). Additionally, the decreased immune response that can take place over time as a result of chronic stress, can lead to periodontal (gum) disease and possibly even trigger the outbreak of cold sores. (Friedman 2019).
Mental health - Depression
According to the World Health Organization (WHO), depression is a common condition worldwide, affecting more than 300 million people. “Depression is different from usual mood fluctuations and short-lived emotional responses to challenges in everyday life. Especially when long-lasting and with moderate or severe intensity, depression may become a serious health condition” (Mental Health of Older Adults, WHO, 2017). Over a lifetime, stressful life events can influence the onset and course of depression.
It’s true that mental health status can have a negative impact on physical wellness, but the opposite is true as well. The presence of poor health and chronic physical conditions can have a direct effect on mental health as well. For example, older adults with health conditions such as heart disease have higher rates of depression than those who are healthy. “Additionally, untreated depression in an older person with heart disease can negatively affect its outcome” (WHO, 2017).
Unmanaged chronic stress can wear down the brain’s ability to function properly, increasing the activity level in the brain’s fear center, potentially causing even greater stress. Over time, electric signals in the part of the brain associated with memory and stress control can start to deteriorate. This process can act as a negative feedback loop, spiraling us into higher levels of anxiety and stress.
Sustained stress interferes with the levels of hormones and neurotransmitters in the brain. When the chemical systems of the body are working normally, they are able to regulate biological processes like appetite, energy and sleep function, as well regulating mood and emotion. However, when the stress response continues over an extended period of time, failing to shut down and reset, it can lead to an increased incidence of depression in some individuals.
Indeed, exposure to unrelenting long-term stress can lead to major depression and anxiety disorders, which are true collapses of multiple brain systems.
Medina, 2018
Ongoing stress can cause depression in older adults. Although depression is not uncommon among the older adult population, it is not a normal part of aging. Depression can affect how we think and feel, and can even affect appetite and sleep patterns. Stress management strategies can help seniors regain emotional balance before it leads to long-term depression, empowering them to take control of their mental and physical well-being.
Longevity
Who doesn’t want a long, healthy life? Recent studies show that one of the keys to longevity may be curbing your chronic stress. In addition to contributing to obesity, heart disease, depression, unhealthy lifestyle behaviors and a host of other conditions, there is now mounting evidence that unmanaged long-term stress can contribute to accelerated biological aging.
Long-term stress has been associated with shortened telomeres. Telomeres have been compared to the plastic tips on shoelaces because they keep the ends of chromosomes from fraying, protecting our genetic information. Telomere length is a marker of both cellular aging and biological aging (Damjanovic, et al., 2007). As telomeres shorten, their structural integrity decreases causing cells to age faster and to die younger.
